A 40 YR OLD MAN WITH SHORTNESS OF BREATH , JAUNDICE & REDUCED URINE OUTPUT
A 40 yr old male patient came to the casualty with CHEIF COMPLAINTS of shortness of breath worsening since 2 hrs ( GRADE 3-4 ) , palpitations, bilateral pedal edema - pitting type since 10-15 days , Abdominal distension & decreased urine output since 15 days , history of fever 1 week back now it was subsided.
HISTORY OF PRESENT ILLNESS:
## Normal routine before this catastrophe , of this 40 year old gentle man was waking up at 6 am and eat food ( rice & curry ) — goes to do work related to agriculture (paddy field worker ) and daily wage worksby 8am — lunch ( rice & curry ) at 2/3 pm — resume work — comes home by 5-6 pm in the evening— takes bath & have dinner ( rice & curry ) — goes with friends outside and have toddy and whiskey — comes home by 9pm .
* He studied 10th class
* He has mixed diet and his married life was 10 yrs , the interaction with the family( wife , two sons : one aged 8 yrs and other 1 1/2 yrs ) was good and he has adequate sleep .
Patient was apparently asymptotic 6 months back ,
One day (6 months back) when he was lifting bricks ; he experienced shortness of breath for the first time and also he noticed some pedal edema
— for which he visited local doctor and was releived of his symptoms and he was diagnosed to have LIVER FAILURE ? ,with yellowish discolouration of eyes and was advised medication , from then he had intermittent episodes of SOB on doing work and continued medication.
* From 6 months his routine remained unchanged ( except he used to take rest and medication when there is an episode of SOB , on doing work ) and he stopped drinking alcohol with his friends , instead of that he spent some quality time with the family.
** But now on presentation ; he developed sever SOB ( grade 3-4 ) again on doing work in the field .
* History of pedal edema, in both lower limbs since 10-15 days which is incidious in onset and gradual in progression and worsened to the present size.
* History of abdominal distension, since 10-15 days which is progressively increasing.
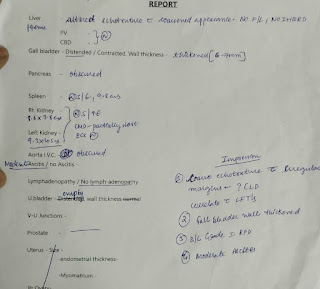
* Endoscopy was done and grade 1 varices are present and ultrasound showing mild splenomegaly.
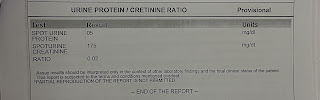
* History of decreased urine output since 10-15 days, with normal stream & post voidal residue with urgency and hesitency present.
## Now his routine changed to an extent that he can’t even walk properly with out developing SOB , so he stopped doing his agricultural and other works, now although he is waking up at 6 am ; he is taking rest , he is having decreased appetite & sleep was normal , family interactions are healthy. The financial needs now ( as he stopped working ) are met by the savings of the family .
PAST HISTORY:
* He is a known case of diabetes since 6 months and was on treatment
* Not a known case of Hypertension, Asthma, TB, Epilepsy, Coronary Artery Disease.
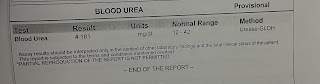
* History of hemodialysis in outside hospital in the view of metabolic acidosis and decreased urine output.
PERSONAL HISTORY:
* Appetite: decreased
* Diet: mixed
* Sleep : adequate
* Bowel and bladder movements: ## Regular bowel movements but,
## Has decreased micturition since 10-15 days
* Additions: * History of toddy intake since 16 years of age & whisky and brandy 90-180 ml since 10-12 years.
FAMILY HISTORY:
* Not significant
GENERAL EXAMINATION:
Patient is conscious coherent and cooperative.
He is well oriented to time, place and person.
He is moderately built and well nourishedVITALS:
Temperature: Afebril
Pulse Rate: 78 beats per minut
Blood pressure: 90/80 mm of HG
Respiratory Rate: 24 cycles per minut
SpO2: 94-96 % on room a
Pallor : present
Icterus : present (mild )
No Cyanosis
No Clubbing
No Lymphadenopathy
Edema : present
SYSTEMIC EXAMINATION:
1) Abdominal examination:
Inspection:
* Shape of the abdomen: distended
* Umbilicus: slit shaped
* No visible pulsations
* Movements of abdominal quadrants with respiration are not appreciated .
* No visible scars.
Palaption:
* No local rise of temperature
* No tenderness
* No palpable masses found
* Liver and spleen are not palpable
Percussion :
* Shifting dullness : present
* Liver span: normal
Ascultation:
* bowel sounds are heard.
2) Respiratory system:
* Bilateral Air entry present
* Normal vesicular breath sounds are heard
* Position of trachea : central
* No wheeze, no crepts
3) CVS:
* S1 and S2 heart sounds are heard
*No murmurs
4) CNS:
* No abnormality detected
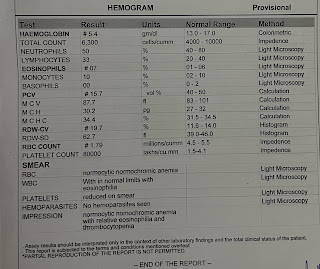
INVESTIGATIONS :
RFT , LFT , HEMOGRAM , CUE , ECG , USG - Abdomen , BGT , ABG , VIRAL SEROLOGY , CHEST X RAY, 2D echo.
Fever chart :